JACKSON ? As is her habit, Cathy Moore called out as she made her way through the kitchen toward the living room where her mother lay in a hospital bed.
“Hey, Puddin’, how are we today?” she asked, using her nickname for 92-year-old Willie Mae Dunlap, whose eyes fluttered in recognition of her daughter’s arrival.
Moore and her brother, Melvin Moore, who have spent much of their lives since 2018 caring for their mother in her Jackson home despite a progressive form of palsy that’s claimed her mobility inch by inch.
Doing so has come with a substantial cost: thousands of hours and thousands of dollars. Melvin, 66, is facing a bill of several hundred dollars to place a wheelchair ramp outside the home. Cathy Moore, 71, has an aching back from months of lifting and carrying her mother.
“It has been up and down emotionally. A lot of people would like to tell you what to do, but they are not going through it,” Cathy Moore said.
It can be lonely work, but they have plenty of stressed-out, financially strapped company across the state. Nearly 1.3 million Michiganders ? more than 10 percent of the state population ? serve as uncompensated caregivers for relatives, spending an estimated $7,000 a year apiece, according to AARP Michigan.
Statewide, the total economic value for such unpaid care is $14.5 billion per year, according to the advocacy group.
The situation is getting worse.
By 2030, those older than 75 will increase to 13.3 percent of Michigan’s population from 7.5 percent in 2020, according to state data. At the same time, national projections predict the pool of potential family caregivers to shrink from seven relatives per senior in 2015 to four in 2030, making it harder for the elderly to stay in their homes.

“Families still provide the majority of care,” said Clare Luz, a gerontologist and professor at Michigan State University’s College of Osteopathic Medicine.
“But there are fewer and fewer family caregivers. We saw this coming, but we had our head in the sand. We are in big trouble.”
A national survey by AARP suggests minority groups bear more of the load, as African-American caregivers report providing 31 hours of care each week and Hispanic caregivers 26 hours weekly, compared to 21 hours by whites.
Michigan already suffers from a gap of paid home care workers, with an estimated shortage of 34,000 direct care workers out of a current workforce of 120,000. The shortage could stretch to more than 200,000 workers by 2026 as more workers leave the field, according to PHI, a New York City-based policy and advocacy nonprofit.

Given those projections, family caregivers in Michigan likely will have to dig even deeper to fill the void.
“I don’t know how this aging population is going to be taken care of,” said Michigan demographer Kurt Metzger, retired founder Data Driven Detroit.
“This whole idea of aging in place and staying in your home and hoping to have someone take care of you ? the numbers just aren’t there.”
‘It’s my mom’
Cathy and Melvin Moore know well that numbers aren’t on their mother’s side.
They grew up in the Jackson home with their mother, Dunlap, and have done their best to cope as she gradually lost mobility over the past three years.
Several months ago, when their mother could still walk with help, the pair struggled to guide her upstairs to a second-floor tub where they could bathe her. At one point, Melvin and his wife, Jennifer, lugged his mother up the steps cradled in a blanket like a makeshift hammock.

Melvin Moore moved from Louisville in the fall of 2018 to his childhood home to look after his mother, even as his wife now lives in a separate apartment in Jackson. To help meet expenses, Melvin does word-of-mouth auto repair from a garage across the street.
“She always took care of me when I was little. It’s my mom,” said Moore, who broke down in tears as he said he “never imagined” he would be changing his mother’s diapers.
Cathy, who retired from a management job some 15 years ago, said the years looking after her mother have prompted worries about her own financial security.
“Sometimes I think I need to get a part-time job, but I just can’t do that now,” said Cathy Moore.
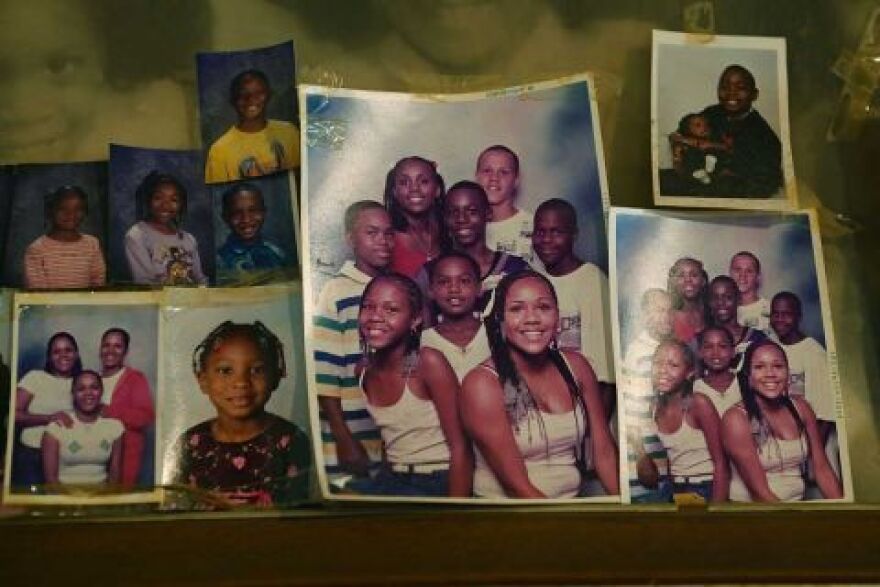
Their mother’s bed is surrounded by scores of photos of her extended family, a legacy that includes eight children, 21 grandchildren, nearly three dozen great-grandchildren and 17 great-great grandchildren.
And while her mother can only speak with great effort, Cathy explained: “She understands everything. Her mouth opens and you have to read lips to understand what she is saying.”
Not long ago, as Cathy bid goodbye, her mother managed to speak these words aloud:
“I love you.”
Michigan spends less to keep elderly in homes
The Moores are grateful for any outside help they now get.
An aide comes for an hour a day to wash and dress their mother, a nurse visits once a week and four hours of temporary relief from a home care aide, known as respite care. The services are funded through Medicaid and the Jackson County Department on Aging.
“That’s all we have right now,” Cathy said.
Advocates say programs to help older adults “age in place” in their homes — rather than go to nursing homes – are woefully underfunded.
The federal Older Americans Act allocates $2 billion per year to states for home-delivered and congregate meals, in-home assistance, preventive health services, transportation, including about $186 million for caregiver support.
Michigan’s projected share for family caregivers is projected for 2021 at just under $5.8 million ? which doesn’t go far with more than a million unpaid caregivers.
Overall, according to a 2020 analysis by AARP, Michigan ranked 30th in the nation in overall long-term care services, including funds for home and community-based care. It ranked 23rd in support for family caregivers.
The analysis, based on data from 2016, found that Michigan spent 31.5 percent of Medicaid funds for long-term care on home and community-based services for older people and adults with disabilities.

Most neighboring states spent more to keep older adults in their homes. Ohio spent 37.1 percent on home and community-based care, while Wisconsin and Illinois spent more than 50 percent and Minnesota spent nearly 70 percent. (Indiana, in contrast, spent 18.4 percent of Medicaid funds on home and community care.)
Lisa Cooper of AARP Michigan said it makes sense to expand state support for home-based care because studies show that it costs the same to care for one person in a nursing home as it does to care for three who live in their homes.
“We know that if a person needs supports and services, they overwhelmingly prefer to receive those in their homes. We can save taxpayer dollars,” Cooper said.
Respite care — a vital lifeline to caregivers who need a break — is available through nonprofit, government and private agencies, and comes in the form of in-home care or drop-off care at adult day centers.
Families who don’t qualify for Medicaid have the option of paying for respite care themselves. But at costs of about $30 an hour for in-home respite care and $100 a day at an adult care center, expenses mount quickly.
“It’s better than nothing,” said Julie Alicki, a licensed therapist who leads support groups for family caregivers in Kent County and former consultant on aging issues to the Area Agency on Aging of Western Michigan.
“But for someone providing care 24-7, especially for someone dealing with Alzheimer’s, it doesn’t touch what they need.”
Caregivers can also turn to community support groups that can be an emotional lifeline, including those for those dealing with family members with dementia and Alzheimer’s.
Medicaid, the state-federal program that helps with costs for people with limited income and resources, pays for in-home care for recipients who meet its income guidelines and who would otherwise qualify for nursing home care.
In Michigan, a program called MI Choice provides home and community-based services for about 15,000 Medicaid beneficiaries each year. The program has a waiting list of 1,800.
Under its guidelines, a married partner of a spouse applying for Medicaid can retain assets excluding the primary residence of about $130,000.
AARP Michigan backs a proposal to add $6.3 million in state funds to the MI Choice program for the fiscal 2022 budget, which would add about 1,000 more slots.
Nicholas Ryan, a Grand Rapids attorney who specializes in elder law, said his firm often hears from clients desperate for help navigating the complexities of Medicaid funding formulas.
“We have clients coming in saying, ‘I’m running out of funds.’ They are at the burnout point, where they are burning the candle at both ends. The family picture I see the most is where adult children are taking care of a parent. The time they are taking for the parent is time they are not taking at work.
“They are literally doing this at the financial detriment of themselves.”
‘Why am I doing this?’
A state official also said many caregivers fail to reach out for help until they are desperate, either out of pride or because they don’t know where to look for assistance. AARP Michigan offers a detailed resource guide for family caregivers, listing a variety of state, local and nonprofit resources to support them.
“Making sure people are aware of the programs that can help is something we are forever working on,” said Lacey Charboneau, field services representative for the state Aging and Adults Services Agency.
The toll can be especially steep for 500,000 in Michigan who care for a loved one with Alzheimer’s disease or dementia.
According to a national report on unpaid caregiving by the Alzheimer’s Association:
- Nearly 60 percent of caregivers rate the stress of caregiving as high or very high. Up to 40 percent report depression
- 16 percent took a leave of absence from work
- 9 percent quit work
Sitting in the dining room of her northern Kent County home, Debbie Burton said she barely considered bringing in outside help as she tended to her husband of 24 years, Jimmy, over the past four years.
“I was really the only person looking after him,” said Burton, 69.

Like many family caregivers, she fell into this role with no training about four years ago, as her husband struggled with diabetes and Alzheimer’s.
“Twenty-four years ago, he made me promise that I would keep him in the house instead of putting him in a home if it ever came to that,” she said.
That came at a cost.
In their previous home, Burton ferried his meals to him in an upstairs bedroom where he spent most of his time. She estimates she made that trek up to 10 times a day, in addition to changing his adult diapers and washing him down in the shower.
“I personally have arthritis and bone-on-bone pain in my knee,” she? said. “It hurt like crazy going up those steps.”
Two years ago, the Burtons moved into a one-level home that Debbie hoped would ease the physical demands of his care.
But by then, the progression of his Alzheimer’s led to jarring shifts in his personality. That sometimes obscured the fond memories Debbie held of their marriage, highlighted by trips to Las Vegas, pontoon boat tours with friends at a Kent County lake, playful times with grandkids.
“There were times when he was mean to me. Here I am doing everything I can for him, and he was yelling things to me, that he hated me. I would say to myself, ‘Why am I doing this?’ I thought I would actually go first, because I was so exhausted and in so much pain.”
At the end of March, Jimmy, 77, died at a Grand Rapids hospital after a fall at home.
Only weeks before that, Debbie Burton finally considered applying for caregiver assistance through Medicaid and joining a caregiver support group. She was reluctant during the COVID-19 pandemic to bring in outside paid care to ease her caregiving tasks.
“I didn’t want strangers coming into our home,” she said.
But she also recalled wedding vows that had guided her through this time.
“When I made the vow, I said in sickness and health,” she said.

East of Ludington, Eric Dolson moved back from Arizona to the family home in November to tend to his aging mother and father, Robert and Lorli Marie.
He did so after he was laid off from a job in financial sales, as he decided to abandon his search for another job to take on this role.
When he moved in, his father was in relatively good health. His mother, however, had battled emphysema for years, and more recently, lung cancer that had spread. Doctors consider the conditions terminal.
Near the end of April, Dolson’s father called out for help from a bedroom.
He was in the midst of a stroke. He died two days later, at 88, in a Ludington hospital after being removed from life support.
Sitting at the kitchen table in the farmhouse that was the family home for decades, Lorli Marie, 87, said she’s grateful for the way her family of nine children rallied to her side.
Her memories spooled back to the decades she and her husband spent tending to their 280-acre fruit farm, back to her high school marching band, and then to childhood recollections of skating in Wisconsin on a frozen lagoon with her parents.
She returned to the present, wondering aloud what she would have done these past few months without Eric. With warmer weather at hand, and flowers blooming, she treasures their short strolls in the yard outside her house.
“He doesn’t replace my husband. But he has been a godsend here. How do you measure something like that?”
As it turned out, Eric was the family member to tell his mother that her husband of 67 years had passed away. At that news, his mother nearly collapsed at the kitchen sink, as she clung to its edge and cried out:
“Who’s going to take care of me?”

This story was produced through the New York & Michigan Solutions Journalism Collaborative, a partnership of news organizations and universities dedicated to rigorous and compelling reporting about successful responses to social problems. The group is supported by the Solutions Journalism Network.
The collaborative’s first series, Invisible Army: Caregivers on the Front Lines, focuses on potential solutions to challenges facing caregivers of older adults.
Correction: This story was corrected to remove an inaccurate attribution of pay increases for direct care workers to SEIU contract negotiations. The pay increases were in fact largely due to legislative action to increase the minimum wage across the board for all Michigan workers.




